Acas Carotid
- Acas Trial Carotid
- Acas Trial Carotid Stenosis
- Acas Carotid
- Acas Carotid Study
- Acas Carotid Trial
- Acas Carotid Study
Carotid arterial stenting (CAS) is a minimally invasive endovascular interventional procedure that can potentially offer the same advantage as surgery (carotid endarterectomy).
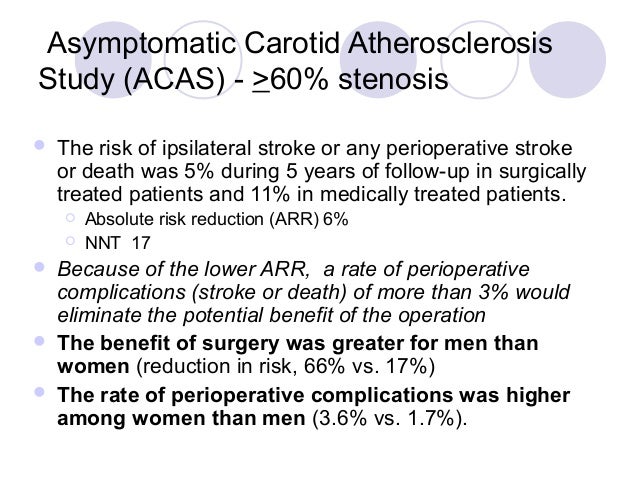
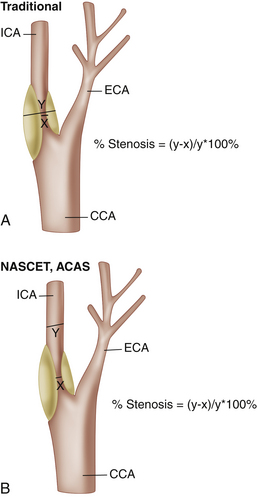
The ACAS31 evaluated the combined use of carotid endarterectomy, aspirin therapy and medical risk factor management in patients younger than 80 years who had asymptomatic carotid artery stenosis. BACKGROUND: Medical therapy for asymptomatic carotid artery stenosis (ACAS) may obviate the carotid revascularization, according to recent literature reports, but many studies also considered moderate carotid artery stenosis (50-69% NASCET). This study reviews the most recent series of ACAS focusing on ipsilateral transient ischemic attack (TIA. CarotidArteryStenosis Executive Committee for the Asymptomatic Carotid Atherosclerosis Study Objective. P=m- To determine whetherthe addition of carotid endarterectomy to. The ACAS established that carotid endarterectomy is beneficial to patients without symptoms and stenosis ≥60% with a postoperative stroke plus death rate of 2.3% and that it reduces the 2-year risk for stroke by 53%.
Indications
Indications for carotid stenting are evolving with endarterectomy trials that evaluate the carotid stenosis cutoff values for treatment. Currently, the indications include:
- symptomatic patients with ≥70% stenosis (NASCET trial)
- asymptomatic patients with >60% stenosis (ACAS study)
- symptomatic patients with stenosis of at least 50-69% stenosis
- carotid artery dissection or pseudoaneurysm
Contraindications
- complete carotid occlusion
- major disabling stroke on the ipsilateral side/disabling dementia
- intracranial tumor/hemorrhage
- unstable plaque or thick calcification at the site of carotid stenosis
- extreme tortuosity of the vessel
Complications
Acas Trial Carotid
- preprocedural cerebrovascular accident (~8%) 3
- recurrent carotid arterial stenosis or in-stent restenosis (~6% at 1 year) 4
- hyperperfusion syndrome after carotid artery stenting (1-2%): headache, seizures and intracranial hemorrhage 6
Alternative treatment options
Outcomes

Operator skills and experience have a profound impact on patient outcomes following CAS. One systematic review and meta-analysis of the literature found Carotid Endarectomy (CEA) to be superior to CAS in freedom from stroke/death within 30 days of treatment, with the incidence of stroke/death within 30 days of treatment was 4.7% for CAS and 3.5% for CEA 8.
Acas Trial Carotid Stenosis
History and etymology
Acas Carotid
- the first percutaneous transluminal carotid angioplasty (PTA) was performed by Charles Kerber in 1980 5.
- somewhat surprisingly the word 'stent' is actually an eponym, originally named after Charles Stent (1807-1885), a largely-forgotten British dentist. He invented an improved material for forming dental impressions and set up a company to manufacture it. During the Great War, J F Esser, a Dutch surgeon used a mold of Stent's Compound as a fixative for skin grafting in injured infantrymen. This innovative use was rapidly adopted into practice, and stenting as a concept rapidly segued into multiple specialties 7.
Acas Carotid Study
- 1. Baerlocher MO, Stewart B, Asch MR et-al. Performance of carotid stenting, vertebroplasty, and EVAR: how many are we doing and why are we not doing more? A survey by the Canadian Interventional Radiology Association. Can Assoc Radiol J. 2008;59 (1): 22-9. - Pubmed citation
- 2. Sacks D, Connors JJ. Carotid stent placement, stroke prevention, and training. Radiology. 2005;234 (1): 49-52. doi:10.1148/radiol.2341041628 - Pubmed citation
- 3. Pelz D, Andersson T, Soderman M et-al. Advances in interventional neuroradiology 2005. Stroke. 2006;37 (2): 309-11. doi:10.1161/01.STR.0000201436.30248.ec - Pubmed citation
- 4. Gröschel K, Riecker A, Schulz JB et-al. Systematic review of early recurrent stenosis after carotid angioplasty and stenting. Stroke. 2005;36 (2): 367-73. doi:10.1161/01.STR.0000152357.82843.9f - Pubmed citation
- 5. Liistro F, Di Mario C. Carotid artery stenting. Heart. 2003;89 (8): 944-8. doi:10.1136/heart.89.8.944 - Free text at pubmed - Pubmed citation
- 6. Karapanayiotides T, Meuli R, Devuyst G et-al. Postcarotid endarterectomy hyperperfusion or reperfusion syndrome. Stroke. 2004;36 (1): 21-6. doi:10.1161/01.STR.0000149946.86087.e5 - Pubmed citation
- 7. Stenting. (2001) Surgical Endoscopy. 15 (4): 423. doi:10.1007/s004640080116 - Pubmed
- 8. Zhang L et. al. Systematic Review and Meta-Analysis of Carotid Artery Stenting Versus Endarterectomy for Carotid Stenosis: A Chronological and Worldwide Study. (2015) Medicine. doi:10.1097/MD.0000000000001060 - Pubmed
Promoted articles (advertising)
Acas Carotid Trial
Acas Carotid Study
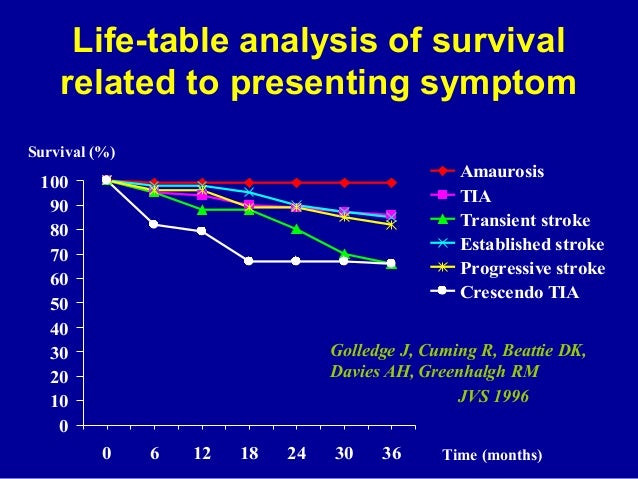
53% relative risk reduction in favor of surgery.1 Cervical atherosclerosis produces stroke by 1 of 2 methods. Arterial thrombosis or particulate atherosclerotic matter may
embolize from the neck lesion to an artery in the brain, producing an ischemic stroke. Second, the atherosclerosis/ thrombosis may progress beyond a critical point, which leads to hypoperfusion of distal vessels, resulting in ischemic stroke. Under these circumstances, survival of the ipsilateral cerebral hemisphere would depend on adequate collateral circulation.
We hypothesized that patients with a contralateral carotid occlusion would be at an increased risk for stroke. Theoretically, these patients would have decreased collateral flow and pressure, and thus embolic and thrombotic events would be more apt to lead to cerebral infarction. In an effort to test this hypothesis, we compared the outcomes of ACAS patients who did and did not have a contralateral internal carotid artery occlusion at baseline.